How Change Management in EHR Implementation Operates

7 Mins
Updated: February 17, 2025
Published: February 1, 2024

Adopting a new EHR solution or overhauling your system is a complex process for leaders and employees. Change management in EHR implementation is key to ensuring the new system is successfully adopted.
As of 2021, according to Health Information Technology 78% of office-based physicians and 96% of non-federal acute care hospitals in the US have adopted a certified EHR.
Electronic Health Record (EHR) systems constantly add new features to simplify workflows, save costs and boost productivity. As a result, healthcare providers are moving to newer platforms or improving current software to maintain care standards.
In this guide, we'll explore the features and benefits of an EHR system, the challenges involved in implementing it, and the crucial role a change management strategy plays in achieving success.
The Basics of EHR
An Electronic Health Record (EHR) is a digital version of a patient's paper chart. EHR systems or software enable different healthcare providers to have instant access to patient-centered records in real time.
The key features of an EHR are:
- Comprehensive data collection – Includes a patient's medical history, diagnoses, medications, treatment plans, allergies, radiology images, and laboratory test results.
- Access and sharing – Enables secure sharing of real-time records, making information available to authorized users across different healthcare environments, such as clinics, hospitals and labs.
- Support for care – Assists healthcare providers in decision-making by providing tools for analyzing patient data and incorporating evidence-based solutions into patient care.
- Patient tracking – Enables EHR tracking of track data over time from multiple visits and providers, making it possible to monitor improvements or deteriorations in patients' health conditions.
These features make EHR a foundational component of modern healthcare infrastructures, enhancing patient care, efficiency, data security and coordination. When deployed effectively, they can significantly improve healthcare operations and patient care.
However, installing or upgrading EHR systems can be challenging for many reasons, including a lack of user buy-in, inadequate training, change saturation and financial issues. These issues can increase employee resistance to the new system and hinder adoption.
Addressing these challenges requires following an effective change management model. With the Prosci Methodology, organizations can develop a detailed plan to launch an EHR system, leading to significant long-term benefits for healthcare providers and patients.
Benefits of EHR Implementation
Here are six primary advantages of using an EHR system:
- Improved patient care – Electronic records provide immediate access to complete patient histories, lab results and medications. This helps clinicians diagnose patients and define a treatment process more efficiently.
- Enhanced coordination of care – Using EHR software, everyone involved in a patient's care can quickly share updates, diagnoses and treatment plans. This is especially crucial for patients with complex chronic conditions.
- Increased patient participation – Many EHR systems allow patients to access their records directly and communicate with care providers. This access helps patients better understand and follow their treatment plans.
- Efficiency and cost savings – EHRs streamline administrative tasks like scheduling, billing and compliance reporting. They also reduce paperwork and prevent repetitive tests, lowering operational costs and improving healthcare delivery.
- Improved data security and compliance – Digital records are easier to secure and back up than paper records, reducing the risk of data loss. EHRs also have advanced security features and audit trails that facilitate compliance with regulations.
- Analytics – EHRs can aggregate vast amounts of anonymized patient data for medical research and population health management. This data is crucial to track public health trends, manage outbreaks and improve healthcare policies.
Overall, EHR implementation makes healthcare safer, faster and more patient-centered. It improves daily operations, enhances public health, and reduces healthcare costs. But deploying an EHR system has its hurdles.
The Challenges of EHR Implementation
Healthcare organizations face five common challenges during electronic health record implementation:
EHR Implementation Challenges

1. Resistance to change
Resistance from clinical teams and other staff is a significant barrier to installing a new electronic health record system.
Healthcare has a unique culture with deeply ingrained practices and norms. Medical practitioners often resist changes that disrupt their established ways of working. They can also be wary of shifts in work routines and habits caused by the new system.
Overcoming resistance requires a robust change management process that includes clear communication plans, employee engagement activities, and visible leadership support.
2. Training and usability
Each EHR system has different features and levels of user-friendliness. Poorly designed interfaces or complex features can lead to user frustration, decreased productivity, and potential errors in patient data management.
Users often need a lot of training to get comfortable with the new system. However, this is difficult because the fast pace of the healthcare industry can shorten the time available for change initiatives.
There can also be disruptions in healthcare delivery and reduced efficiency during technology implementation as users become familiar with the new system, impacting patient throughput and satisfaction.
3. Resource and cost constraints
Healthcare providers often face constraints in both monetary and non-monetary resources for EHR implementation. This includes software and hardware acquisition, infrastructure upgrades, consulting fees, and training.
After installing the new system, they also have ongoing costs related to system maintenance, software updates and potential upgrades to compete with evolving healthcare standards and technologies.
Change teams can struggle to get funding for EHR initiatives, especially if the organization has multiple change projects underway.
4. Regulatory and compliance challenges
Healthcare is a heavily regulated industry. Since EHR systems store sensitive patient information, they must comply with strict regulatory requirements for data security, patient privacy and healthcare quality standards. Additionally, EHR software must also support reporting and audit functions.
These regulations can be demanding and add complexity to the implementation process.
5. Change saturation
Healthcare organizations often face multiple simultaneous changes. In addition to adding or upgrading EHR systems, changes related to organizational restructuring or new regulations are common.
Healthcare organizations often face multiple simultaneous changes. In addition to adding or upgrading EHR systems, changes related to organizational restructuring or new regulations are common.
The cumulative effect of constant changes can lead to change saturation and change fatigue, where staff feel overwhelmed by the volume and pace of changes. This can increase resistance from a burned-out workforce.
Many healthcare organizations are at or past the point of change saturation, and the trend continues across industries. In the Prosci Best Practices in Change Management research, 73% of respondents said their organizations were near, at or beyond the saturation point.
Level of Change Saturation

Addressing these challenges requires a well-defined change management strategy. This strategy involves thorough planning, stakeholder engagement, continuous training, and a focus on the technical and cultural aspects of change.
Using Change Management for Successful EHR Implementation
Effective change management is critical in navigating the challenges of implementing an EHR system and ensuring that the organization, staff and patients benefit fully from the new technology.
Success requires pulling in the right resources, sponsors, people leaders, and others within the healthcare institution to help implement the recommendations. Here’s a high-level look at how a change management practitioner can guide each step.
1. Establish a clear vision and leadership commitment
Change management helps develop a compelling vision for EHR implementation, emphasizing its benefits. Change practitioners help key stakeholders create a shared definition of success, aligning the change with organizational goals.
Strong leadership commitment is crucial for driving change. Sponsors are responsible for ensuring the change achieves the desired outcomes. They champion the EHR initiative, regularly communicate the vision and progress to stakeholders, and allocate necessary resources. They can also secure essential funding and navigate constraints.
Prosci research shows active sponsorship is the most important contributor to change success.
Contributors to Success Over Time

Effective change management also includes support from change practitioners who equip sponsors for their role in change, including actions to ensure alignment with organizational goals.
2. Engage and support stakeholders
Effective change management involves diverse stakeholders in planning and decision-making. Including doctors from different departments, clinical staff, IT personnel, technical staff and patients builds support for the EHR implementation and helps minimize resistance behaviors.
Because upgrading or installing a new EHR system directly impacts these employees and their daily work, keeping them involved in the change helps them feel ownership.
Using an individual change model like the Prosci ADKAR® Model is an indispensable tool for helping people move through the change process successfully.
Prosci ADKAR Model
For example, clinical managers use our ADKAR Model to help staff adopt and use the new EHR system, coach them through barriers, and even identify and resolve their own resistance.
3. Develop technical integration and training programs
Using our ADKAR Assessment, change teams identify skills gaps as part of their change management strategy. They can then develop customized training programs for different user groups to ensure that all staff are competent and comfortable using the new EHR system.
During the planning stages, change practitioners and stakeholders can work together to evaluate the compatibility of the EHR system with their existing healthcare infrastructure. Using this information, they can create an implementation plan that outlines how the EHR system will integrate with other systems and technologies.
Organizations must also provide continuous learning opportunities and a support system, including help desks and user manuals, to assist employees during and after implementation. Support mechanisms must include dedicated technical staff to manage integration challenges and provide ongoing assistance.
4. Optimize workflows and minimize disruptions
Following a structured approach, like the Prosci 3-Phase Process, helps teams understand how EHR implementation will impact people and processes, and strategize accordingly. It also enables organizations to analyze and redesign existing workflows for improved performance.
During implementation, change teams roll out the new system in phases, starting with a pilot phase to refine workflows and address issues.
Implementing changes in phases allows employees to adapt gradually and tackle issues as they arise, compared to an instant large-scale disruption that can impact productivity, disrupt workflows, or introduce errors in patient records.
5. Address change saturation
Hospital leadership can work with change teams and stakeholders to mitigate the negative effects of change saturation and maintain staff satisfaction. They must create a project inventory or change portfolio to prioritize change initiatives and use a change framework to facilitate the transition.
The Prosci Methodology
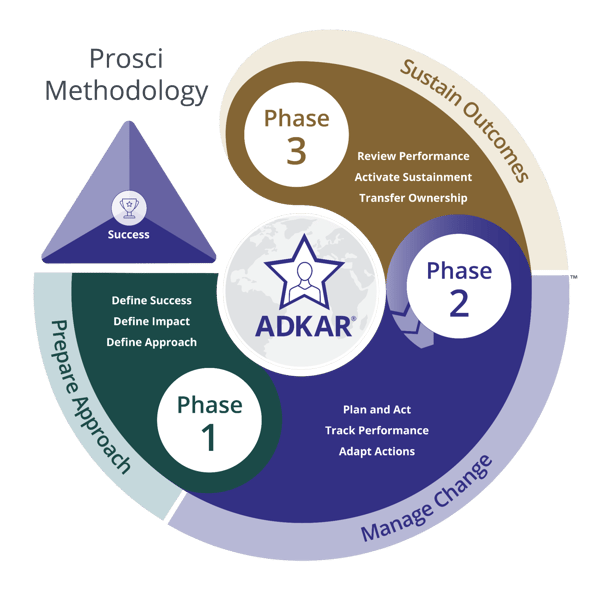
The Prosci Methodology is a structured approach to change management that helps organizations manage the people side of change and avoid overwhelming staff.
Organizations can use this methodology to understand how change impacts healthcare workers and prioritize change projects to avoid overwhelming them. By focusing on high-priority projects, leaders and employees get the time and resources they need to implement changes that align with overall business goals.
Focus on the people side of change to drive successful organizational change and avoid change saturation, considering how change can affect employees’ responsibilities.
6. Ensure regulatory compliance
Change management includes planning for regulatory compliance before, during and after implementation. Businesses can involve legal and compliance experts early in the change process to ensure all changes meet industry regulations.
While preparing a change strategy, organizations can embed compliance requirements into the EHR system's design and implementation processes. The strategy can also allocate time and processes for maintaining detailed documentation and records. This facilitates regulatory audits and ensures ongoing compliance.
Proactive compliance planning prevents costly and time-consuming legal issues and reinforces the organization's commitment to maintaining high standards of care.
7. Plan for long-term sustainment
Change management builds in long-term planning and tactics to ensure that adopting the EHR changes stick over time. Without reinforcement, employees will likely revert to older systems or processes after initial adoption.
Reinforcement activities like continuous feedback, visible performance measurement, rewards and recognition for adopting the EHR system, and celebrating milestones can help employees stick with the new operational processes.
Your change strategy can also address the technical side of reinforcement, like creating a maintenance plan for regular updates and performance optimization. It can also involve nurturing partnerships with EHR vendors to support long-term efficiency through system upgrades and technical assistance.
Prosci Elevates EHR Implementation
Through meticulous planning and strategic change management, healthcare organizations can use EHR systems to revolutionize patient care. However, major challenges during EHR implementation can disrupt operations, hinder adoption and lead to change saturation. A structured change management approach ensures that organizations effectively adopt the EHR system, achieving the best results for both patients and team members.